How We Can Help
We partner with Medicaid managed care organizations (MCOs) to deliver well-child exams in MedExpress centers. When children who are enrolled in a Medicaid plan visit our center, we offer to perform a well-child exam at that time. Health education and guidance is provided for all well-child visits and covers age-appropriate guidance on topics from nutrition and dental care to sleep and physical activity. And after each exam, we can send a comprehensive report to the MCO’s case management department to help ensure proper care coordination.
We provide dedicated training for our staff and medical providers that is customized to each health plan’s needs and requirements. This training includes scripting to explain the importance of a well-child exam and the process that will take place.
Since MedExpress began providing well-child exams, we’ve conducted more than 40,000 youth wellness screenings across eight states.
Well-Child Partnership Benefits
MedExpress is uniquely positioned to help increase access to care because of our convenient hours and locations as well as our walk-in care model. By partnering with us, you can further improve health outcomes for your youngest Medicaid-covered lives and increase referrals to primary care providers for needed follow-up care.
Our partnership can help you to increase the reach of patients served, so you can meet state Medicaid quality metrics and improve your overall HEDIS scores.
Access to Local Care
youth wellness screenings in 8 states, convenient locations, extended hours
Improved Quality Metrics
Increase patient reach, meet Medicaid metrics, improve HEDIS scores
Close Gaps in Care
Case management reports, care coordination, referrals to PCPs
Customized Solutions
Staff and provider training, patient education, nutritional counseling
Serving the Underserved
Children covered under Medicaid tend to face obstacles to getting the care they need. It is estimated that less than half of the children between ages 12-21 who are enrolled in Medicaid receive a well-child visit.1 Additionally, according to the Office of the Inspector General, 51 percent of randomly sampled Medicaid providers were not available for appointments. This same study found that the providers who were available for appointments had a median wait time of two weeks; 10 percent had wait times longer than two months.2
West Virginia
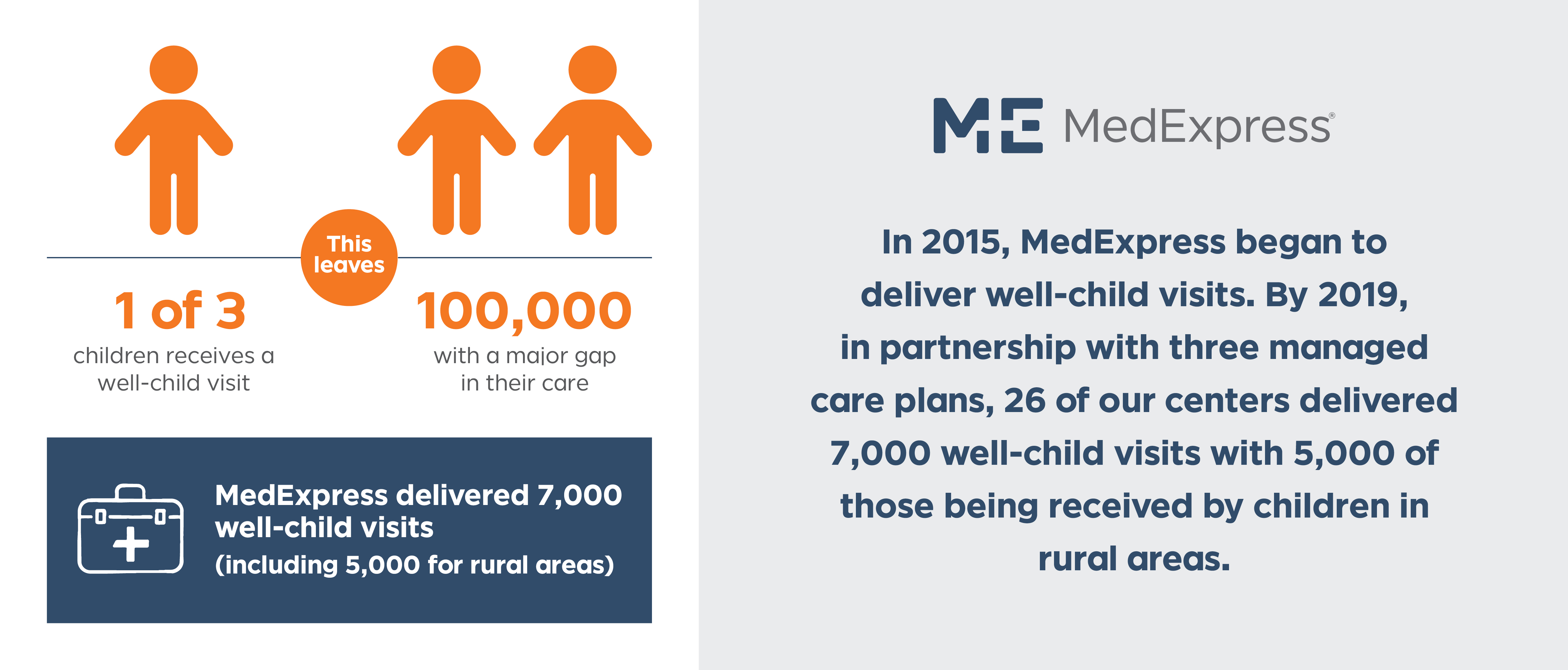
In this state, just one in three Medicaid patients from the ages of 3 to 18 receive a well-child visit. This leaves 100,000 children with a gap in their primary care each year.3
In 2015, MedExpress began to deliver well-child visits. By 2019, in partnership with three managed care plans, 26 of our centers delivered 7,000 well-child visits with 5,000 of those being received by children in rural areas.3
Together we can help make access to well care easier for Medicaid-covered children and their parents, and together we can help improve outcomes for this underserved population.
let's talk
For more information, please contact us.
Sources:
1 U.S. Department of Health and Human Services. 2014 Annual Report on the Quality of Care for Children in Medicaid and CHIP. Last updated November 2014. Accessed December 19, 2018.
2 U.S. Department of Health and Human Services, Office of Inspector General. Access to Care: Provider Availability in Medicaid Managed Care. Last updated December 2014. Accessed December 19, 2018.
3 Optum analysis conducted in 2020.
